LATE ONSET IUGR STAGES STAGE BASED MANAGEMENTS , what is after Gratacos stage based managements for early onset IUGR
Abstract
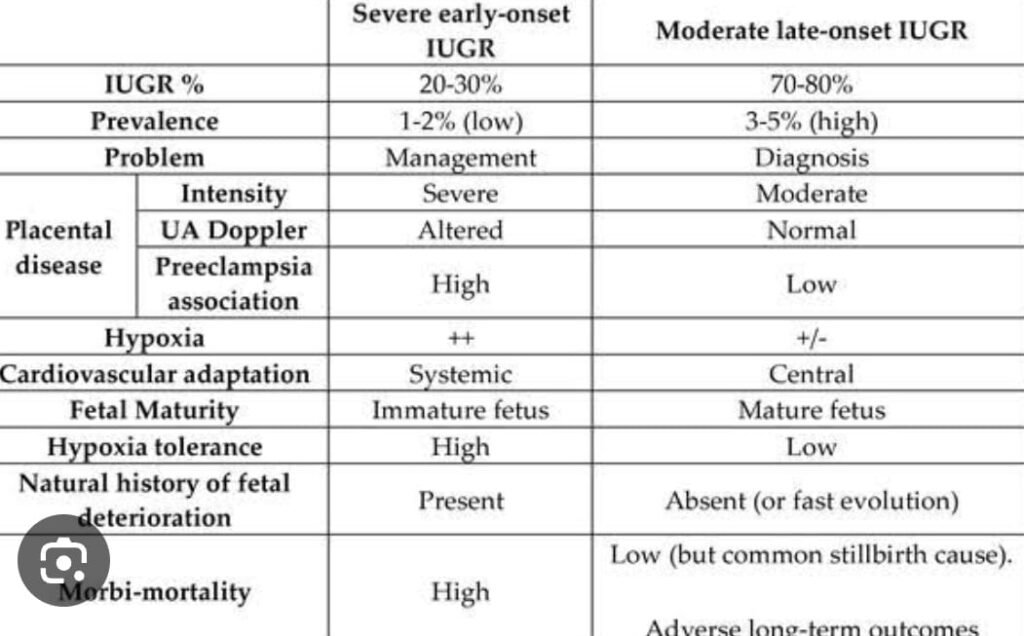
Intrauterine growth restriction, regarded as one of the great obstetric syndromes, represents a serious obstetric condition that can lead to increased perinatal morbidity, mortality and postnatal impaired neurodevelopment. There are two main distinct phenotypes of IUGR: early onset and late onset with different ages of onset, patterns of evolution and fetal Doppler profiles. It has been noted that many of the so-called “unexplained” stillbirths in the late 3rdtrimester are appropriately grown fetuses. Therefore new definitions and concepts have been added to the diagnosis of IUGR including failure to reach growth potential (FRGP) and intrafetal growth restriction (IFGR). Implementation of these new definitions aim to improve and widen the detection of fetal compromise, moving away from considering only size as the main diagnostic parameter for compromise, to hypoxia.
The two pathophysiological concepts relating to placental intrauterine growth restriction are anomalies in placental intervillous perfusion and anomalies in placental intervillous diffusion, which ultimately determine the clinical phenotypes of early and late onset IUGR. In early onset IUGR the anatomical defect is in the spiral arterioles, while in late onset IUGR the anatomical effect is at the level of the villi. The degree of the abnormal perfusion or diffusion influences the arterial Doppler pattern which is used as the main diagnostic tool in monitoring.
In early onset IUGR the main Doppler modifications are at the level of the umbilical artery with progressived eterioration of the pulsatility index until absent or reversed end diastolic flow is reached. The changes in the cerebral, cardiac and ductus venosus circulations follow a sequential and predictable pattern to severe fetal compromise. In lateonset IUGR the middle cerebral artery pulsatility index (MCA PI) and the cerebroplacental ratio are the main parameters for both diagnosis and to plan management whilst the umbilical artery pulsatility index is generally normal.
In all cases of IUGR the ultimate aetiology relates to an interplay of the fetal genotype, maternal phenotype and genetic-environmental interactions. Early onset IUGR is generally a management problem whilst late onset IUGR is mainly a diagnostic challenge. Patterns of deterioration of IUGR have been identified which allows for an integrated and scientifi c approach to the management.
Introduction
Intrauterine growth restriction is a complex obstetric condition that can have a maternal, fetal or placental aetiology or can occur due to a combination of these factors. This is review will deal mainly with IUGR of placental aetiology, in the absence of obvious primary maternal or fetal factors, and will address recent developments in definition, diagnosis and management.
There are different types of placental IUGR and different criteria has been developed to define these.1,2,3 The most widely accepted definitions of IUGR are the following:
- Classical Early Onset IUGR: when the abdominal circumference (AC) or fetal weight (FW) is p95 for gestational age at gestational age < 32-34 weeks
- Classical Late Onset IUGR: when the AC or FW 32-34 weeks
- Failure to Reach Growth Potential (FRGP): here fetuses are generally between p10-p50 (so these fetuses technically are in a so-called “normal fetal weight range”) but are compromised ie these fetuses are in an hypoxic or low oxygen environment. These fetuses may have MCA Doppler anomalies or CPR
- Intra fetal Growth Restriction (IFGR): here the fetus serves as its own control. In this scenario growth restriction is diagnosed when the AC and/or FW cross centiles by > two quartiles on growth charts on tracking –irrespective of where the percentile is. IFGR may also be diagnosed where there is static growth or tailoring of growth over a period of time.
Pathogenesis
There are two pathophysiological concepts relating to placental intrauterine growth restriction, namely abnormal placental intervillous perfusion and abnormal placental villous diffusion.
These abnormalities usually are specific to the two main types of IUGR. Early onset IUGR is generally related to anomalies in placental intervillous perfusion whilst late onset IUGR relates to anomalies related to placental villous diffusion. In both cases the core pathophysiology is placental but the anatomical defectvaries; in early onset IUGR the anatomical defect is in the spiral arterioles ;in late onset IUGR the anatomical effect is in the villi. In both cases the ultimate aetiology relates to an interplay of fetal genotype, maternalphenotype and gene –environment interactions.
Intervillous perfusion refers to the high nutrient and oxygenate dmaternal blood arriving at the intervillous space, which then has to diffuse into the fetal circulation via a process of villous diffusion. Normal placental vascular transformation ensures a low resistance, high materno-placental system which is sonographically determined by a low resistance or pulsatility index in the uterine arteries matched with a low umbilical artery resistance or pulsatility index.
In early onset IUGR there is a lack of or inadequate placental vascular transformation which results in the establishment of a high resistance low flow materno-placental system. The uterine artery pulsatility index shows changes early in the process and thus can be used as a screening tool in the prediction of early onset IUGR in both the first and second trimester risk assessments. The maternal perfusion is therefore challenged due to high systemic pressures and the resultant low materno-placental blood flow can result in placental ischaemia and necrosis, which in turn results in significant areas of the placenta becoming non-functional.
Early onset IUGR is categorised by early placental failure which allows time for fetal adaptation to develop in response to a hostile environment resulting in low metabolic demands and therefore has a longer latency to demise.
In late onset IUGR there is generally normal perfusion but altered diffusion. There is centralisation of the fetal circulation as an immediate feature in response to hypoxia and there are consequences to this in that a reasonably growing fetus with a mature brain is now exposed to a low oxygen environment. Furthermore this is an acute process due to acute placental failure and the consequence of this is that the fetus is now at an increased risk for neurobehavioral developmental anomalies and an increased stillbirth risk.
Late onset IUGR is secondary placental failure in a scenario where a reasonably grown fetus is subjected to an acute process of failure ; so in effect a fetus with already reasonably high metabolic demands is placed in the environment of acute restriction and therefore there is a short latency to fetal demise.
Diagnosis
Early onset IUGR is almost exclusively linked to a lack of placental vascular transformation and placental maladaption between 8-15 weeks gestation leading to a sequence of events that manifests phenotypically as IUGR in the late 2nd trimester or early 3rd trimester. We can tract the cascade of cardiovascular deterioration (generally) quite precisely by looking at alterations in flow velocities by Doppler especially in the umbilical artery (UA), progressing from an elevated UA PI >p95 to absent end diastolic flow (AEDF) to reversed flow (REDF), abnormal cardiac function, abnormal cerebral circulation and leading finally to ductus venous Doppler anomalies. At this stage the fetus is in a hypoxic and/or acidotic state and generally when there is reversed flow in the umbilical artery and venous Doppler anomalies there will be major fetal compromise within three to five days.
In early onset IUGR the premier tracking vessel in monitoring the condition is thus the umbilical artery.
In late onset IUGR, all these screening and diagnostic tests perform poorly and this is especially true for the umbilical artery blood flow velocities which is unpredictable.
The reason for this poor sensitivity is that, contrary to popular belief, the UA PI will only detect fetal compromise when 30% or more of the placenta is non-functional. When this occurs, it translates into an umbilical artery Doppler anomaly, but this is unlikely to happen in a reasonably well developed placenta in late onset growth restriction. The reduction of placental capacity (which is a reduced diffusion capacity) may impact on fetal growth but may not be enough to translate into a umbilical artery flow velocity abnormality.
The MCA PI is needed to distinguish between a late onset IUGR scenario with its consequences, from a possible constitutional small fetus.
Late onset IUGR can only be diagnosed by the a small for gestational age fetus (though not always) and MCA PI 11-13 To complicate matters further, the fetus in late onset IUGR may not always be small.
In late onset IUGR the premier tracking vessel is the middle cerebral artery in which there could be abnormality in flow in response to hypoxia i.e. increased flow to the brain as a neuroprotective mechanism and therefore a reduced PI of
In late onset IUGR the following findings are usually detected after 32 to 34 weeks gestation:
- • Normal Umbilical Artery Doppler Indices
- •Arterial Redistribution as reflected in the MCA PI < p5 for GA
- Then increased PI more than 95 centile
- • Abnormal Cerebro-Placental Ratio (MCA PI/UA PI)
- • Normal Venous Doppler
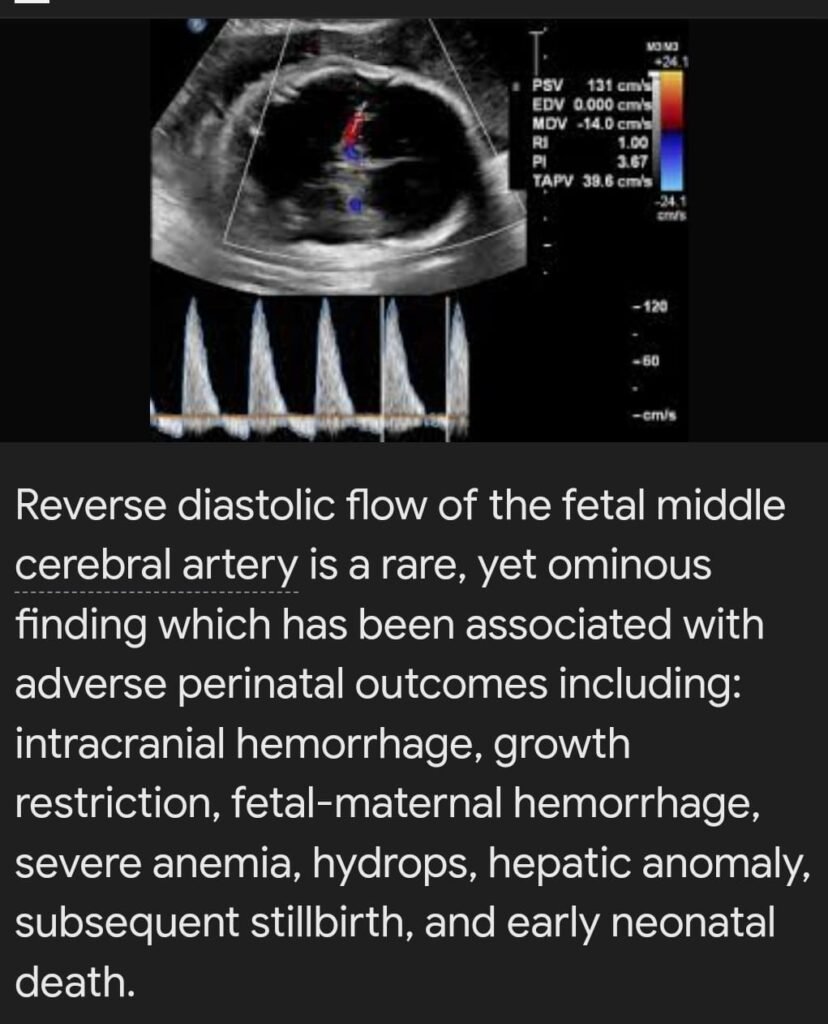
- reversed diastolic flow
- intrasystolic notching
- Cardiovascular deterioration seldom beyond cerebral circulation
Management of Early Onset IUGR
If a diagnosis of early onset IUGR is made, the clinician needs to decide how often to monitor the fetus. In order to make this decision, scientific evidence is needed to establish and predict the patterns of deterioration of IUGR. three patterns have been identified in the progression of early onset IUGR, which relates to when and how it started. The gestational age of onset of the IUGR and the rate of deterioration of the UA PI in the first 7-10 days after diagnosis is used to predict the rate of cardiovascular deterioration. three rates of progression have been described namely severe, progressive or mild.
Gestational Age of Onset around 26 to 28 weeks
Patients who present between 26-28 weeks gestation with IUGR and severe worsening of the umbilical artery Doppler in the initial 7-10 days, predicts progression to venous Doppler anomalies within 14 daysthat may result in very early intervention. Follow up should be three times per week and this scenario will most likely result in delivery close to 30 weeks gestation.
Gestational Age of Onset around 30 weeks
The progressive path will generally refer to cases diagnosed close to 30 weeks with mild deterioration in the UA PI within 7-10 days of diagnosis, and depending on the cerebral circulation and venous circulation delivery is likely at 33-34 weeks.
Gestational Age of Onset around 32 weeks
The mild IUGR pathway generally refers to the IUGR diagnosis at 31-32 weeks and where the umbilical artery Dopplers have not deteriorated in the initial 2 weeks from diagnosis, and is unlikely to do so. The mild path of deterioration is categorised by flow anomalies confined to the umbilical and cerebral circulations. Delivery is often at 36-37 weeks.
Before 34 weeks the chronic hypoxia path to stillbirth occurs with absent end diastolic flow ( AEDF) occurring two weeks before, and reversed end diastolic flow (REDF) occurring a few days before the adverse event and is therefore precisely predicted (Fig 2).
Management of Late Onset IUGR
After 34 weeks, acute placental failure results in acute hypoxia with deteriorating MCA and CPR being the strongest predictors for stillbirth The acute nature of the hypoxia does not leave time for other fetal Dopplers to get abnormal.
Late onset IUGR is generally not a management problem but rather a diagnostic one. The two main factors that drive management in late onset IUGR is risk of neuro behavioural development anomalies and the risk of still birth. Each case has to be individualised as different variables maybe present in the clinical scenario which is also dependent on the degree of the MCA and CPR anomaly present. Generally, however in late onset IUGR delivery by 37 weeks is appropriate or earlier depending on other variables.
Discussion
If the prediction of adverse outcome continues to depend only on sizeof the fetus in the 3rd trimester, we will certainly fall short and miss the majority of compromised fetuses. This is demonstrated by a large study by Vasak et al in the Netherlands, who tracked a million term births over a 6-year period, and recorded 5075 perinatal deaths. Although the small for gestational age fetuses as a group had the biggest number of stillbirths(fetal weight <p10) , the largest number of stillbirths was recorded infetuses with fetal weights in the 10th to 50th centile for gestational agegroup which by definition were not small for gestational age. After 36 weeks, an astonishing 72% of stillbirths were >p10 for gestational age. This again demonstrates that late fetal compromise often occurs in fetuses who are in a so-called “normal range fetal weight”. The challenge is how would we identify these fetuses.
The main issue surrounding IUGR is not often about size but all about hypoxia. By introducing broader definitions of IUGR, the focus is allowedto be re-orientated. Such concepts as “Failure to Reach Growth Potential (FRGP)” and “Intra-Fetal Growth restriction (IFGR)” are therefore useful in that the definition of IUGR moves away from size to hypoxia as theprimary diagnostic parameter for fetal compromise.
Conclusion
Many late 3rd trimester stillbirths are labelled as “unexplained” when in reality these fetuses were hypoxic but were missed. This is related to gaps in definition and the lack of sensitive fetal parameters to adequately address the devastating problem of late 3rd trimester stillbirths. Future research should be directed at developing models to adequately predict and diagnose fetal hypoxia in the late 3rd trimester. Such models need to move towards a combined model incorporating multiple parameters such as biometry, the cerebro-placental ratio, cardiac function and possibly a serum or blood biomarker (sFlt-1 or placental growth factor or both).
we propose in addition to Gratacos based classification for IUGR which is mainly focusing on early onset IUGR MANAGEMENT STAGE BASED CLASSIFICATION , We do propose a late onset IUGR STAGE based classification
we will depend mainly on MCA Doppler as it will measure the diffusion for the fetus from placenta which is the main concern for the fetus in late onset IUGR , could the cause of impaired diffusion be diabetes or hypertension or unknown cause in most of cases
, stage I is showing high diastole and MCA PI less than 5th centile
stage ii increased systole mca PI more than 95 th centile
STAGE IIII appearence of intrasystolic notching in mca systole with indices more than 95th
stage iv for immediate delivery with high pi and reversed diastolic flow